Immunological memory following SARS-CoV-2 infection
How does immunological memory develop? How well does it protect against re-infection and how is it formed in long Covid?
Covid-19 is an immense challenge for society as a whole and for healthcare systems in particular. Intensive care for people with severe forms of the disease and providing care for people living with the long-term consequences of Covid pose formidable demands for medicine. Onur Boyman’s research group at Zurich University Hospital is investigating how immunological memory forms after a SARS-CoV-2 infection, how it protects the body against reinfection and what its characteristics are in people with long Covid.
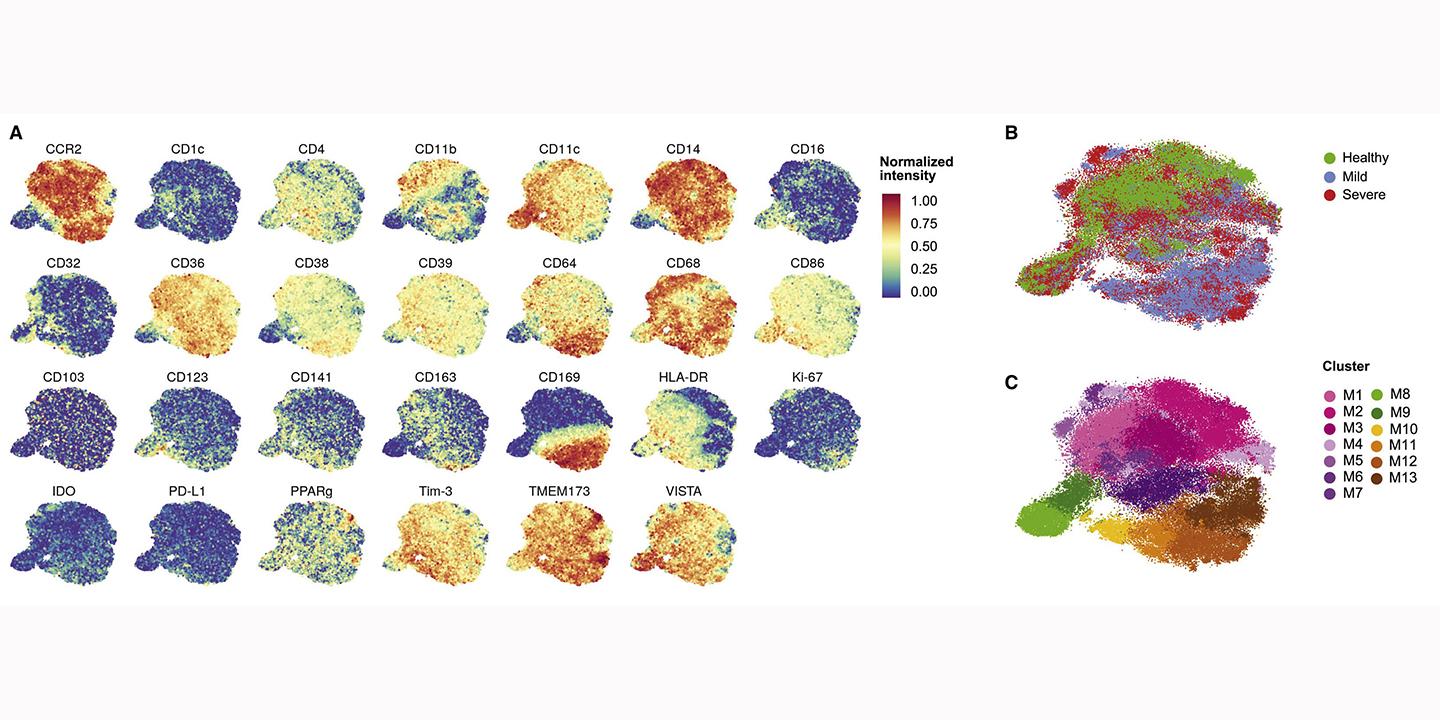
By conducting regular blood sampling and clinical check-ups of patients with various long and severe forms of the disease, they have now obtained their first findings. Since the study started over a year ago, acute immune response to SARS-CoV-2 infection or vaccination and the formation of immune memory have been tracked in 215 participants. This manifests in the establishment of various immune responses. In particular, the scientists are tracking the effect and development of humoral, cellular and innate immunity.
For example, the severity of an individual’s Covid-19 is reflected in their humoral – i.e. antibody-mediated – immune response. In some mild, asymptomatic cases only a local neutralisation of the virus in the mucous membranes is initiated, whereas in severe cases – which occasionally end in acute lung failure – the blood often contains large quantities of antibodies. This goes hand-in-hand with high levels of inflammatory cytokines, which remain elevated for a period of more than 40 days from disease onset. Cytokines are messenger substances in the immune system that influence immune response.
Cellular immunity can also change dramatically during the acute phase of severe Covid-19 infection. For example, the composition of the T-cell population may be altered, with redistribution in the body and with T-cells dying off in some cases. Hence the low T-cell counts observed by the researchers. This process is also associated with elevated levels of inflammatory hormones.
The researchers are currently analysing the T- and B-cells which specifically recognise the SARS-CoV-2 virus in patients’ blood up to a year after they contracted it. These research results will improve our understanding of how people with the disease develop immune memory – something that is of particular interest, given the potential threat posed by new variants of the virus.
In a follow-up study, the researchers are investigating how the development of immune memory in people after a SARS-CoV-2 infection differs from that in people who have been vaccinated against SARS-CoV-2. Furthermore, they are examining patients who have developed PACS – post-acute Covid-19 syndrome, or “long Covid” – following infection. Going forward, this knowledge could help doctors adapt the treatment of patients who are dealing with the long-term consequences of Covid-19.
Publications